Abdominal aortic aneurysms (AAA)
Last edited on : 22/09/2024
Abdominal Aortic Aneurysm (AAA) is a dilation involving all layers of the arterial wall with an anteroposterior diameter greater than 35 mm in men and greater than 30 mm in women (some consider a 30 mm limit regardless of gender). The prevalence is ~1% in men aged 55-64, and it increases by 2-4% every 10 years. Depending on the series, it is present in 3 to 8 men for every woman and is slightly more common in Caucasian populations. It is usually asymptomatic or minimally symptomatic, often discovered incidentally. Management varies from simple monitoring and risk factor treatment to prevent progression, to surgical or endovascular repair. Complications are generally severe. The preferred location is infrarenal (with extension to the iliac arteries in up to 50% of cases), which is at the highest risk for complications.
Etiologies and Risk Factors
These are the same as for any aneurysm (see specific chapter). However, AAA is primarily caused by atherosclerosis in the vast majority of cases.
Clinical Presentation and Discovery Circumstances
- Most are asymptomatic or minimally symptomatic, sometimes discovered incidentally:
- Imaging for digestive, urinary, or lumbar pathologies
- Abdominal palpation: pulsatile expanding mass (pushing the hands with each systole, very suggestive), sometimes with a bruit; De Bakey sign (the ability to slide the edge of the hand between the superior pole of the mass and the costal margin = highly suggestive of an infrarenal aneurysm)
- Symptomatic in case of complications, see below
- Particular presentation of inflammatory AAA (formation of perianeurysmal fibrosis that can extend to neighboring organs and/or envelop non-aneurysmal aortic segments):
- Abdominal or lumbar pain, weight loss, anorexia, general deterioration, fever, nephritic colic, lower limb edema
Most cases are discovered incidentally or during complications (++ with rupture). Without complications, they may (especially in cases of rapid growth) cause minimal and nonspecific symptoms (abdominal pain, lumbosacral pain, urinary disturbances), misleading the practitioner toward a lumbar or digestive workup.
Natural Evolution
- The increase in diameter is highly variable (individual variability + depending on the starting diameter), but on average ~2.5 mm/year.
- The risk of rupture depends on wall tension = Pressure x Radius / Wall thickness (Laplace’s Law). Risk factors include:
- Maximum diameter:
- 40-49 mm → 1.3%/year
- 50-59 mm → 5 to 10%/year
- 60-69 mm → 10 to 20%/year
- 70-79 mm → 20 to 40%/year
- Rapid diameter increase (significant risk if >5 mm/6 months)
- Uncontrolled hypertension
- Maximum diameter:
Complications and Associated Conditions
Rupture of Abdominal Aortic Aneurysm
A severe complication, which can occur spontaneously or after even minimal trauma or exertion, can present in different forms:
- Fissure ("pre-rupture") and dissection → acute lumbar pain, stable hemodynamics, tender pulsatile mass... a nonspecific clinical presentation often leading to an incorrect diagnosis until a full rupture occurs.
- Retroperitoneal rupture → acute lumbar pain, pulsatile mass on palpation, hypotension and tachycardia (sometimes transient) before the onset of collapse → overall mortality ~50%
- Intra-peritoneal or hollow organ rupture (rare, involving the duodenum, small intestine, colon, inferior vena cava) → usually presents as sudden death or severe sudden collapse → overall mortality >90%
Overall, the mortality rate for AAA rupture is nearly 100% without proper intervention and, if the patient is admitted alive to the emergency room, the mortality rate is 20 to 50% with appropriate management.
Compression of Neighboring Organs
- Compression of the inferior vena cava → lower limb edema, rarely thrombosis
- Ureteral compression → lumbar pain, urinary disturbances, nephritic colic
Thromboembolism
See the detailed article: Mesenteric Infarction, Ischemic Colitis, and Abdominal Angina
See the detailed article: Acute Limb Ischemia
Depending on the site: "blue toe syndrome," lower limb ischemia, renal infarction, mesenteric infarction, etc.
Potential Complications Specific to the Underlying Etiology
Associated Conditions
They depend on the underlying cause. However, in the vast majority of cases, it is related to atherosclerotic disease. Additionally, a popliteal aneurysm is found in 15% of patients with AAA.
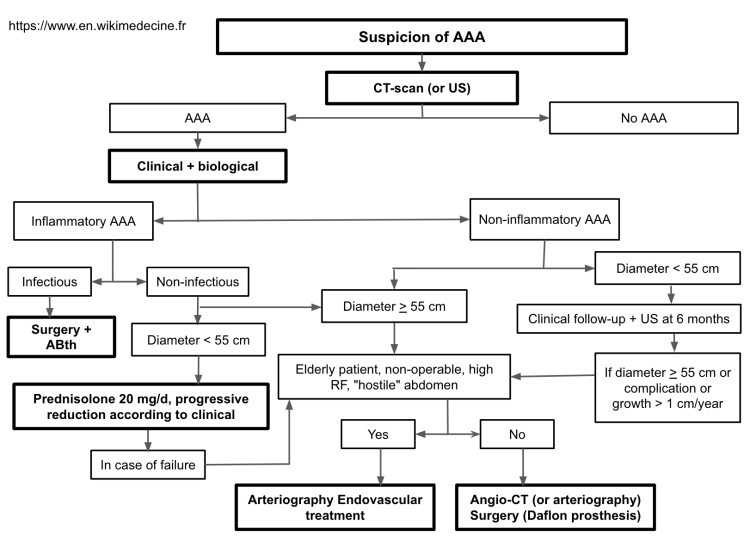
Additional Examinations and Management of Uncomplicated Abdominal Aortic Aneurysms
The mortality rate for conventional surgical repair is low (~4-8%), and complications (pseudoaneurysms, infections, or graft thrombosis) are rare. The mortality rate for endovascular treatment is 1.4%, and complications are even more limited. However, the cost is higher, long-term data is still lacking, and anatomical constraints (such as contraindications in cases of short neck, iliac or aortic tortuosity) are significant.
The use of β-blockers has been proven effective in Marfan syndrome patients. However, their administration in other patients not undergoing surgical treatment remains a topic of debate.
Etiological treatment should be applied when necessary.
Depending on the underlying cause, associated pathologies must be investigated. An ultrasound to check for popliteal aneurysms is systematically justified.
The above protocol is, of course, only a proposal to be adapted to the practices of the reference center. Some consider a diameter of 50 mm as the threshold for intervention. After an uncomplicated intervention, angiographic monitoring is recommended at 1, 6, and 12 months, then annually.
Management of Ruptured AAA
A ruptured AAA is always a surgical emergency (Dacron graft) or an endovascular repair depending on the hospital center's level of expertise. Pre-surgical supportive care is usually required (fluid challenge and transfusions in case of hemorrhagic shock, without exceeding a MAP of 70 to 80 mmHg; prioritize β-blockers and avoid direct vasodilators in cases of hypertension, following the model of thoracic aortic dissections). Use this time to confirm the diagnosis with an ultrasound before proceeding with surgery.
Bibliography
Chung J, Epidemiology, risk factors, pathogenesis, and natural history of abdominal aortic aneurysm, UpToDate, 2024
Dalman RL et al., Management of asymptomatic abdominal aortic aneurysm, UpToDate, 2024
Dalman RL et al., Overview of abdominal aortic aneurysm, 2024
Jim J, Clinical features and diagnosis of abdominal aortic aneurysm, UpToDate, 2024
EMC, Traité d'Angéiologie, 2018