Carcinomatous meningitis
Last edited on : 30/08/2024
Carcinomatous meningitis or meningeal carcinomatosis is a tumoral meningitis defined as hematogenous meningeal infiltration by neoplastic cells leading to multifocal meningeal metastatic development. Today, its prognosis remains extremely poor, even with optimal, early management.
Etiologies - Primary cancers
Melanoma (secondary melanoma meningitis), bronchial neoplasia (carcinomatous meningitis occurs during the course of 5-20% of bronchial cancers) and breast cancer account for the vast majority of primary neoplasia. The time between diagnosis of the primary disease and meningitis varies from a few days to over 20 years.
Carcinomatous meningitis is, however, the mode of revelation of neoplastic disease in 10-20% of cases.
Clinical features
Variable association of :
- "Cerebral" signs: variable headaches (exceptionally the only sign present), diffuse encephalopathy, consciousness disorders, neuropsychiatric disorders, hemiparesis, epileptic seizures.
- Signs of cranial nerve damage (present in 50-75% of cases on initial examination)
- Radicular signs (present in ~75% of cases on initial examination, mainly radicular pain, classically bilateral or "rocking")
- Possible cauda equina syndrome
- Meningeal signs, apart from headache, are exceptional.
The association of central and peripheral multifocal signs in a patient with active neoplasia or a history of neoplasia should always raise the suspicion of carcinomatous meningitis.
Differential diagnoses
Cerebral metastases, chemotherapy or radiotherapy toxicity, paraneoplastic neurological syndromes, neurosarcoidosis, chemical tumor meningitis and other causes of chronic meningitis, etc.
Additional tests
Imaging may be normal or show suggestive images, although not pathognomic. In all cases, cerebrospinal fluid analysis is essential for diagnosis.
- CT-scanner injection:
- Usually normal, but may reveal multiple nodular contrasts in the cerebellum and basal cisterns, or a ribbon-like contrast in a cortical gyrus.
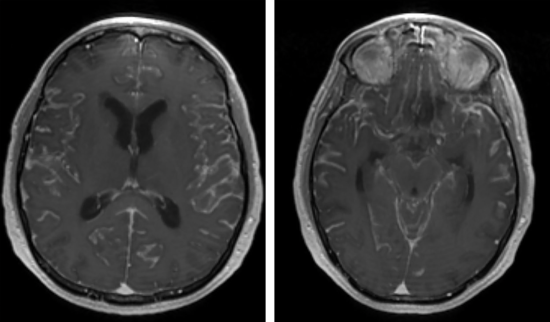
- MRI + gadolinium (whole neuraxis)
- Frequently normal
- Signs possibly suggestive of the diagnosis: signs of chronic meningitis, subarachnoid nodules (hypointense in T1, hyperintense in T2 with gadolinium)
- The main benefit is to eliminate most differential diagnoses.
- Lumbar puncture (LP)
- Cerebrospinal fluid (CSF) almost always abnormal: hyperproteinorachia, hypoglycorachia, rare lymphocytosis
- Cytology positive in 75-90% of cases if performed 2 x → affirms diagnosis
- Immunohistochemistry: useful if cytology negative + arguments for nature of primary.
- Investigative workup in the absence of known neoplasia (careful skin examination, chest CT-scan, PET-scan, mammography, etc.).
Course - prognosis
Progression and prognosis are variable (although generally very poor in the short term, even with optimal management), depending on the nature of the primary neoplasia and how early treatment is initiated. Spontaneous evolution is usually fatal within a few weeks. Irreversible neurological sequelae are the rule if treatment is delayed → Any suspicion of carcinomatous meningitis warrants immediate hospitalization with urgent brain CT-scan and LP + oncological, neurological or neurosurgical opinion as soon as direct CSF examination is performed to plan further workup and therapeutic management.
Therapeutic management - Treatments
- Chemotherapy, example : Intrathecal methotrexate (via PL or intraventricular Ommaya/Rickam reservoir) 12.5 mg 2 x/week +- folinic acid 10 mg 1 x/ 6 hours over 24 hours.
- Intrathecal alternatives to methotrexate: thiotepa (10 mg 2-3 x/week), AraC (25-100 mg 2-3 x/week), depocyt liposomal (50 mg 1 x/ 2 weeks)
- Systemic chemotherapy may be considered if there is a history of panencephalic radiotherapy (destruction of the blood-brain barrier).
- Corticosteroid therapy: intrathecal dexamethasone (5 mg aacidexam) combined with chemotherapy (transient improvement). Essential in case of meningeal reaction to chemotherapy.
- Possible radiotherapy of symptomatic areas
- Classic treatment complications: chemical meningitis, infectious meningitis caused by Staphylococcus epidermidis, etc.
Paramedical support (in such situations, it is generally useful to plan the next stage in advance): support from a psycho-social team, management by a pain or palliative care team within the hospital or at home. In the case of outpatient care, contact the attending physician and encourage him or her to contact a palliative care team at home.
Appropriate management of primary neoplasia when it is found.
Author(s)
Dr Shanan Khairi, MD
Bibliography
Bradley WG et al., Neurology in clinical practice, 5th ed., Butterworth-Heinemann, e-dition, 2007
Cambier J et al., Neurologie, 13e édition, Masson, 2012
Demopoulos A et al., Clinical features and diagnosis of leptomeningeal metastases from solid tumors, uptodate, 2015
Demopoulos A et al., Treatment of leptomeningeal metastases (carcinomatous meningitis), uptodate, 2014
Osborn AG et al, Brain, Elsevier, 2018
Pradat PF, Méningites chroniques, Encycl Méd Chir (Elsevier), Neurologie, 17-160-C-30, 2002