Cerebrospinal fluid - main abnormalities
Last edited on : 7/10/2023
Cerebrospinal Fluid (CSF) is secreted by the choroid plexuses, circulates in the ventricular system and subarachnoid spaces, and is drained through venous resorption via the one-way valves of Pacchioni's granulations.
It serves mechanical (shock absorption), immune, pressure regulation, and transport functions.
A sample can be obtained through a lumbar puncture, more rarely through a surgical device, or exceptionally, directly through a dural breach. Its analysis is a central step in the diagnostic, prognostic, or therapeutic evaluation of many neurological clinical situations.
Technical aspects of lumbar puncture (LP)
An anxiolytic may be considered fifteen minutes before the puncture if the patient is very anxious or confused.
Patient position: lateral decubitus, curled up in fetal position (possibly "helped" by a cushion between the arms). It is preferable to perform the puncture on the patient in the supine position, rather than in the seated position:
- less subject to patient movement during puncture
- the practitioner must become accustomed to performing the puncture with the patient in the decubitus position, as many clinical situations require this:
- sedated or critically ill patients
- the need to measure CSF pressure. Pressure standards are set for a supine patient, and the rules for "correcting" the measurement when puncturing a seated patient are unreliable, depending on the patient's size.
Put on a sterile gown and gloves, disinfect the skin thoroughly, take your bearings and mark the planned puncture point (look for an intervertebral space on the midline at the level of the iliac crests), place the sterile drape.
An anesthetic is usually injected at the puncture site. However, if the practitioner is experienced (good positioning, no iterative trials before successful puncture, thin or atraumatic trocard used), it is not useful: it is the fact of "piercing" the skin that is most painful, as the anaesthetic only has an effect on the superficial layers.
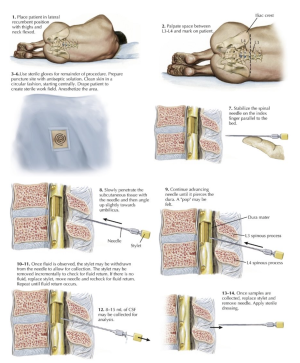
Perform the puncture in a straight line with slight cranial angulation. Ideally, progress is unobstructed until a slight resistance ("click") is encountered before penetrating the subarachnoid space, from which the CSF will flow. Most failures result from :
- Superficial obstruction (spinous process): you are not in an intervertebral space. Withdraw the needle completely and choose a new puncture point +- 1cm above or below, depending on the situation.
- Obstacle 2 or 4 cm deep (vertebral arch blade): you are too paramedian. Withdraw the needle down to the skin and make a millimetre angulation to the left or right via the same puncture point, depending on the situation, possibly upwards.
- Obstacle more than 6 cm deep (vertebral body): you've missed the "click" and passed the subarachnoid space. Gently move the needle back a few millimetres to a centimetre.
- Your needle is fully inserted and you have not encountered any obstacles: you are not on the midline. Withdraw the needle completely and take your bearings again.
When the CSF is flowing, place the pressure column and measure the pressure if indicated, or collect the CSF directly. Usually, 3 tubes of 3 to 5 cc are sufficient. Collect an additional 5-10 cc tube for "refrigerated" storage, if possible. Number the tubes.
Contraindications, Complications, and Indications... of a Lumbar Puncture
Contraindications (relative depending on the severity and clinical probability of the presumed diagnosis):
- Presence of a central nervous system lesion with a significant mass effect or obstructive hydrocephalus
- Proximity of the possible puncture points to a skin infection
- Major hemostasis disorders (always perform a complete blood count and coagulation test in cases of suspected hepatic insufficiency or hematopathy), thrombocytopenia (platelets < 30000/ mm3 or rapidly developing thrombocytopenia), effective anticoagulation. If sampling is essential, seek hematological advice beforehand to correct the disorders as best as possible (platelet transfusions, etc.).
Complications
Cerebral Herniation
- Rare, risk exists in the presence of a lesion with mass effect
- Risk of temporal herniation in cases of supra-tentorial lesion, cerebellar herniation in cases of infra-tentorial lesion. Rapid fatality is the norm.
- Upon suspicion: cerebral CT scan, notify a neurosurgeon (or any senior surgeon in the absence of a readily available neurosurgeon) to consider decompression without waiting for imaging results.
Extradural or Subdural Hematomas
- Exceptional, complications mainly occur in cases of coagulopathy or therapeutic anticoagulation at effective doses
- Risk of cauda equina and terminal cone (medullary) distress. Dark functional prognosis.
- Upon suspicion: spinal cord CT scan (MRI in case of negative CT if Hb < 10 g/dl, as blood may then appear isodense on the scan) → pain relief, correct coagulation disorders, neurosurgical consultation without waiting for imaging results.
Abscesses, Meningitis, and Septic Cerebral Venous Thromboses (CVT)
- Exceptional, by catheter contamination
- Prevention: equipment sterility, disinfection, ensure absence of local infection
Disc Herniation
- Exceptional, on ligamentous lesions
"Post-LP" Headaches
- Frequent, likely due to intracranial hypotension on occult dural breaches
- There are no Evidence-Based Medicine (EBM) on this matter, but certain measures are recommended by consensus to minimize the risk of their occurrence: thin catheter, strict 6-hour post-LP decubitus rest with oral hyperhydration
- Intracranial hypotension clinic (see intracranial hypotension syndrome): dominated by orthostatic headaches with +/- paresthesias, exceptionally observed cranial nerve involvement (traction), nonspecific visual disturbances
- Diagnosis is clinical. An MRI of the neuraxis with gadolinium - often not contributive - is only indicated in cases of atypical clinical presentation and diagnostic doubt.
- No therapeutic EBM, but suggest blood-patch + decubitus rest + pain relievers + hyperhydration. Spontaneous resolution of the syndrome in the following days is the norm.
- Suspect complications of intracranial hypotension (exceptional) in cases of disappearance of orthostatic character or worsening of symptoms:
- Subdural Hematomas
- Cerebral Venous Thromboses
Dermoid Implants
- Rare, with most cases described following the introduction of a catheter without a trocar. Their treatment consists of surgical excision.
Formal Indications for Emergency Lumbar Puncture
- For diagnostic purposes:
- Suspicion of meningitis or meningoencephalitis: lumbar puncture within 30 minutes of admission.
- Performing a lumbar puncture in no way justifies delaying the administration of antibiotics in cases of suspected bacterial meningitis and/or acyclovir in cases of suspected herpetic encephalitis. The analysis of cerebrospinal fluid, including cultures, is not altered in the first 24 hours following the initial administration of antibiotics.
- Systematically perform a cerebral CT scan pre-puncture in cases of presence of focal neurological deficits or signs of intracranial hypertension
- Strong suspicion of subarachnoid hemorrhage (SAH) with normal CT scan
- Suspicion of intracranial hypertension (ICH) with normal cerebral imaging
- Suspicion of acute inflammatory pathology of the nervous system (acute disseminated encephalomyelitis, myelitis, acute polyradiculoneuritis, ...)
- Suspicion of meningitis or meningoencephalitis: lumbar puncture within 30 minutes of admission.
- For therapeutic purposes:
- Lumbar punctures for discharges of 30 to 40 cc in cases of intracranial hypertension in the absence of mass effect (cerebral venous thromboses, idiopathic intracranial hypertension, ...) with visual disturbances or significant headaches or papillary edema resistant to acetazolamide (diamox)
In cases of contraindication to performing a lumbar puncture, surgical sampling of cerebrospinal fluid can be exceptionally considered with a neurosurgeon depending on clinical imperatives.
Characteristics of Cerebrospinal Fluid
Pressure
Normal values for cerebrospinal fluid pressure in lateral decubitus position range from 4.5 to 20 cmH2O. A lumbar puncture should be performed in lateral decubitus to measure pressure. Occasionally used corrections for measurements taken in a seated position are not validated.
Cellularity
- Normal values:
- Leukocytes < 5 to 10/mm3 (approximately 75% lymphocytes and 25% monocytes, absent or rare neutrophils)
- Red blood cells < 10 to 100/mm3.
- In cases of traumatic contamination (common), red blood cells are usually non-crenated, and the leukocyte/red blood cell ratio is similar to the blood ratio (generally 1/1000). Unfortunately, nothing, not even the "three tube technique," allows for a definitive differentiation between traumatic contamination and non-traumatic presence of red blood cells.
- An increase in leukocytes in cases of meningitis depends on:
- Etiology: bacterial, viral, inflammatory, neoplastic, chemical
- Patient's immune status or recent antibiotic therapy (no change in cellularity within the first 24-48 hours of starting antibiotics).
- The presence of neoplastic cells indicates carcinomatous meningitis.
Glucose Concentration (Glycorrhachia)
A cerebrospinal fluid glucose concentration lower than 50% of blood glucose suggests bacterial, tuberculous, Listeria, carcinomatous, or connective tissue meningitis.
Proteins
The normal protein concentration is 0.2 to 0.4 g/L. The origin of these proteins (mainly albumin) is primarily plasma-derived. Elevated protein levels are highly nonspecific, and interpretation should always consider serum protein levels. They may indicate:
- Elevated serum protein levels, confirmed by blood tests.
- Disruption of the blood-brain barrier (hypertension, vasculitis, hemorrhages, meningitis).
- This can be confirmed by measuring the blood/CSF albumin ratio (normally below 6 to 8 x 10-3).
- Protein production by nervous tissue.
- Intrathecal production of lymphoplasmacytic Ig (quantitative/qualitative measurement, more sensitive and specific: search for oligoclonal bands with comparison to plasma). This indicates inflammation, acute or chronic, broadly affecting the nervous system.
- "Albumin-cytological dissociation" (increase in protein concentration without a corresponding increase in nucleated elements) is nonspecific but specifically suggests acute polyradiculoneuritis, spinal cord compression, poliomyelitis, and diphtheric neuropathy.
- Isolated hypergamma globulinemia suggests: multiple sclerosis, neuromyelitis optica, acute disseminated encephalomyelitis (ADEM), spinal cord compression, neurosyphilis, cerebral venous thrombosis, neoplasia, trypanosomiasis, iose, subacute sclerosing panencephalitis, etc.
- Frequent false positives in case of hemolysis with CSF Hb > 1 mg/L!
Appearance
- "Clear as water": normal appearance.
- Yellowish to orange-pink (xanthochromic): indicates hemolysis (presence of degraded red blood cells → bleeding dating back more than 6 hours).
- Pink to red (hemorrhagic): indicates the presence of undegraded red blood cells → bleeding within the last 6 hours.
- Probable traumatic origin if absence of xanthochromic supernatant, presence of bilirubin, and clarification in three tubes. These characteristics, however, do not allow for a definitive distinction between traumatic and non-traumatic origin... thus must be considered in light of clinical suspicion.
- Should raise suspicion of subarachnoid hemorrhage even in cases of normal CT scan, but may also indicate other pathologies: subdural and extradural hematomas, acute disseminated encephalomyelitis, and hemorrhagic meningitis or meningoencephalitis (justifying systematic culture).
Bacteriology
Upon direct examination, the following organisms are particularly to be considered in case of:
- Diplococci:
- Gram positive: pneumococci?
- Gram negative: meningococci?
- Bacilli:
- Gram positive: listeria?
- Gram negative: haemophilus?
Various
The total volume of CSF, V(CSF), is approximately 150 ml on average (renewed 4 times a day).
An elevation of LDH is nonspecific, but in the context of hyperleukocytosis, it should raise suspicion of bacterial glycolysis.
Chloride measurement, which is less sensitive and specific compared to other parameters, is no longer recommended in clinical practice.
Clinical Situations Justifying a Lumbar Puncture
Meningeal Syndrome
The main etiologies are subarachnoid hemorrhages and meningitis. The main differential diagnoses are intracranial hypertension, migraines, and meningeal irritation.
Brain imaging is advisable before performing LP due to clinical overlap between meningeal syndromes and intracranial hypertension. Additionally, it can reveal radiological signs suggestive of encephalitis.
In cases of high suspicion of bacterial or herpetic meningitis, the following approach should be taken:
- Blood sampling and immediate initiation of empirical antibiotic therapy + acyclovir
- Cerebral CT scan
- LP
- Re-evaluation based on LP results
Subarachnoid hemorrhage can be confirmed if cerebrospinal fluid is hemorrhagic, after ruling out hemorrhagic meningitis or traumatic LP.
- Traumatic LP can be suspected based on the following criteria: decrease in hemorrhagic character over 3 tubes, < 1000 RBCs/WBCs, formula similar to that of blood, absence of crenated RBCs, absence of xanthochromic supernatant after centrifugation, absence of bilirubin pigments by spectrometry.
- However, no criteria definitively differentiate between traumatic and non-traumatic origin. In cases of high clinical suspicion of subarachnoid hemorrhage, performing a cerebral angiographic CT scan is justified to rule out the presence of an aneurysm.
- Hemorrhagic meningitis should be suspected if there are more than 4 WBCs/1000 RBCs, low glycorrhachia, fever, immunosuppression, or inflammatory syndrome. Any doubt should immediately lead to or continue with antibiotic therapy + acyclovir.
In cases of persistent doubt, a cerebral MRI (T1, T2, FLAIR, T2*, DWI) should be performed before any potential angiography.
In cases of suspected meningitis, the following elements can provide guidance while awaiting culture, serology, and PCR results:
| CSF | Proteins | Leukocytes | Glucose | Lactate | Direct examination | Cultures |
|---|---|---|---|---|---|---|
| Viral | normal to 1 | < 1000
Lymphocytes > PNN (possible acute majority of PNN) |
Normal
(sometimes low) |
Normal | Negative | Usually negative |
| Bacterial | 1 à 5 | 500 à 10.000
> 50% PNN |
Low
(normal in 10%) |
High | Positive in > 60% of cases | Positive in 90% of cases |
| Tubercular | Increased | 200 à 300 | Low | High | Positive in 25% of cases | 85% positive |
| Standards | < 0.4 g/l | < 5/ ml
(100% lymphocytic) |
> 50% of gylcemia | < 2mEq/ l | Negative | Negative |
In doubtful cases, where cultures and conventional PCR tests come back negative, the demonstration of an absence of intrathecal Ig production (not very specific but very sensitive) is enough to rule out an infectious origin.
Suspected intracranial hypertension (ICHT)
Any suspicion of intracranial hypertension must be preceded by imaging to exclude a mass effect with risk of involvement. In such a situation, LP is contraindicated (to be discussed if bacterial meningitis is suspected). The main etiologies of HTIC are: head trauma, meningitis and other central nervous system infections, cerebral venous thrombosis and other cerebrovascular accidents, tumors, inflammatory diseases of the central nervous system, idiopathic HTIC, etc.
Whatever the etiology, symptomatic HTIC (an alarm symptom being the appearance of visual disturbances) requires treatment (diamox, PL discharges, surgical shunting, optic nerve fenestration, craniectomy, etc.) under neurosurgical responsibility.
Suspected intracranial hypotension
The diagnosis is strictly clinical in the case of a typical form with a clear etiology (post-PL context, symptoms clearly aggravated by orthostatism, absence of neurological deficit). In other situations, or in the absence of improvement despite symptomatic treatment, an imaging scan (clinically similar to an HTIC picture) is performed prior to LP with pressure measurement.
Suspicion of an inflammatory disease of the nervous system
Possible CSF abnormalities are as numerous as they are aspecific: hyperproteinorachia, elevated leukocytes and red blood cells, intrathecal Ig production, etc. Blood abnormalities may also be present in cases of systemic pathology.
Suspicion of chronic adult hydrocephalus
Opening pressure is often in the high normal range (not very sensitive, aspecific). Allows discharge LP for diagnostic and therapeutic purposes.
Author
Dr Shanan Khairi, MD
Bibliography
Cambier J et al., Neurologie, 12e éd., Masson, 2008
Goetz CG, Textbook of Clinical Neurology, 3th ed., Saunders, 2007
Johnson KS et al., Cerebrospinal fluid: Physiology and utility of an examination in disease states, UpToDate, 2021