Mesenteric adenitis (= adenolymphitis)
Last edited on : 24/09/2024
Mesenteric adenitis involves (sub)-acute inflammation of the mesenteric lymph nodes. Ordinary, typical of the child or young adult, its etiology is usually viral (in 80% of cases - Epstein-Barr Virus,...), more rarely bacterial (Yersinia, mesenteric tuberculosis,...) or parasitic (toxoplasmosis, giardiasis,...) exceptionally related to neoplastic or chronic inflammatory disease.
Its evolution is usually self-limiting and does require in most cases only symptomatic treatment. Because of its frequency, and despite its generally "benign" character, this pathology should be known to all general practitioners, pediatricians, internists and emergency physicians, in order to avoid unnecessary and potentially harmful complementary examinations.
It should be noted that, depending on the series published, 10 to 20% of patients undergoing exploratory surgery for suspected acute appendicitis have their diagnosis corrected to mesenteric adenitis on the basis of intra-operative macroscopic or pathological findings.
Clinical evaluation
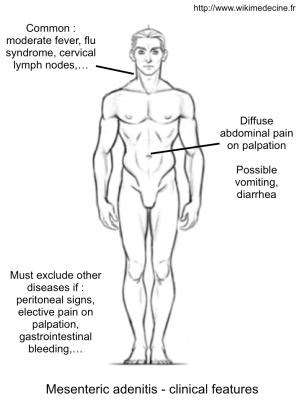
The stereotypical clinical presentation consists of the association of:
- Diffuse abdominal or iliac fossa pain (can mimic appendicitis or diverticulitis) + - vomiting and bowel dysfunction. Generally mimic gastroenteritis (diffuse abdominal pain - vomiting - diarrhea).
- Moderate fever is common.
- Upper respiratory tract infection, presence of cervical lymph nodes or flu syndrome suggests a viral etiology.
In case of viral etiology, pain disappear within a few hours to a few days in most cases. Their persistence, the onset of general deterioration or rapid clinical deterioration have to rule out bacterial infection, complication (intussusception in children) or differential diagnosis (other causes of acute abdominal pain and gynecological etiologies, also inspect the testicles in children and young adults because testicular torsion may start with lower abdominal pain) and think a pharyngitis or pneumonia in case of fever (declaring frequently by abdominal pain in children).
Peritoneal signs are possible but still have to rule out a surgical emergency.
Differential diagnosis
The differential diagnosis of (sub)acute mesenteric adenitis is that of acute abdominal pain, to be modulated according to the clinical presentation. The main confusing diagnoses are appendicitis and diverticulitis.
The rare cases of chronic mesenteric adenitis should lead to discussion of certain infectious (tuberculosis, parasitosis, HIV, etc.), tumoral or inflammatory etiologies (Crohn's disease, ulcerative colitis, hereditary periodic fevers, granulomatous diseases, etc.) depending on the clinical context.
Investigations
If there is no sign of seriousness and no doubt about a surgical pathology (reassuring elements : child or young adult, no peritoneal signs, improved within 3 days, conservation condition, no bloody vomiting or bloody diarrhea, no elective localized tenderness, ...), no further investigation is necessary. In other cases, we realize:
- Blood tests : variable inflammatory syndrome according to etiology
- Pregnancy test, tigette and urinalysis (to rule out renal colic and urinary tract infection)
- Abdominal ultrasound or CT-scan : confirms the presence of supra-centimetric mesenteric lymphadenopathies, evaluate the severity and complications and rule out surgical differential diagnoses.

Management
If typical clinic without any argument for a bacterial etiology :
- Only symptomatic treatment, similar to the treatment of gastroenteritis : paracetamol + - nonsteroidal anti-inflammatory drugs. General measures (diet "gastro", rehydration). No other attitude has demonstrated effectiveness.
- Antiemetics and antidiarrheals are rarely useful in adults and must be avoided in children. Preference for the rehydration per os, with Solutes Oral Rehydration by age, and even consider a brief hospitalization in case of abundant diarrhea and / or vomiting or clinical signs of dehydration in very young children and newborns.
- If necessary, reassure parents (often very anxious and misunderstand the doctor's attitude found negligent about the pain intensity of their child) and explain in what cases represent emergency. Followed in consultation with the attending physician to 72 hours.
In other cases:
- Achieving a emergency radiological imaging is justified only in case of reasonable diagnostic doubt or fear of a complication. If inconclusive imaging : clinical and laboratory monitoring and repeat imaging to 24 hours.
- Antibiotics (++ fluoroquinolone / cyclin) are only justified in cases of bacterial etiology suspicion (deterioration of general condition, high CRP, no clinical improvement over a few days, rapidly worsening).
Bibliography
Carty HM, Paediatric emergencies: non-traumatic abdominal emergencies, Eur Radiol. 2002 Dec;12(12):2835-48
Hawkey CJ et al., Textbook of clinical Gastroenterology and Hepatology, 2d edition, Wiley-BlackWell, 2012
Kliegman RM et al., Nelson textbook of pediatrics, 18th edition, Saunders, 2007
Lambot K et al., Les urgences abdominales non traumatiques de l’enfant, J Radiol, 2005; 86:223-33
Toorenvliet B et al., Clinical differentiation between acute appendicitis and acute mesenteric lymphadenitis in children, Eur J Pediatr Surg, 2011 Mar;21(2):120-3
World Health Organization and UNICEF, Production of the new ORS, WHO Press, 2006
Yang WC et al., Etiology of non-traumatic acute abdomen in pediatric emergency departments, World J Clin Cases, 2013, Dec 16; 1(9): 276–284
NB: this article, the first french version of which was written in 2014, has been, without being referenced, pumped in large part by the Ooreka french website and then by others, copying us or each other, i.e. the passeportsanté and santésurlenet french websites. This is plagiarism, and it's totally inappropriate, even from purely commercial sites.