Neuropathic pain
Last edited on : 22/09/2024
Neuropathic pain is defined as pain caused by a lesion or dysfunction of the nervous system, occurring in the absence of a nociceptive stimulus and unrelated to inflammatory processes.
It may be isolated or associated with nociceptive pain.
Diagnosis
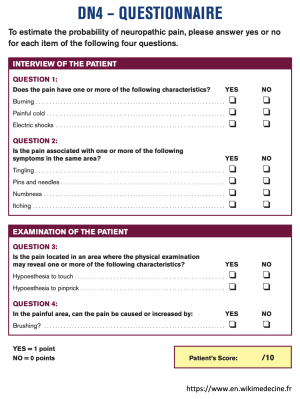
Diagnosis is exclusively clinical, with further investigations only for etiological purposes or to rule out differential diagnoses. DN4 questionnaire (positive if score > 4: sensitivity 83%, specificity 89%):
The presence of objective abnormalities on general examination (e.g., joint or systemic signs) or neurological examination (e.g., motor deficits, hypo- or hyper-reflexia) should prompt consideration of purely nociceptive pain, mixed pain, or a specific etiology of neuropathic pain. The differential diagnosis with psychogenic origins or components is very challenging.
Etiological Investigation of Nervous System Involvement:
- Metabolic: Diabetes, alcoholism, hypothyroidism, chronic renal failure, etc.
- Rheumatologic conditions: Mixed pain within the context of disc-radicular pain, carpal tunnel syndrome, and other entrapment syndromes.
- Neoplastic: Nerve destruction or compression.
- Iatrogenic and radiotherapy.
- Infectious: Shingles, HIV, etc.
- Traumatic: Nerve trunk injuries, brachial plexus avulsion.
- Postoperative: Thoracotomy, inguinal hernia repair, cesarean section, saphenous vein stripping, dental procedures, etc.
- Central origin: Multiple sclerosis, stroke, spinal cord injury, phantom limb, etc.
- Idiopathic and psychogenic: Diagnoses of exclusion.
Management
Etiological Treatment
Essential when possible.
Symptomatic Treatment
First-line:
- Tricyclic antidepressants: e.g., amitriptyline (10-25 mg per night, up to 100 mg/day).
- Contraindications: Cardiac disorders, glaucoma, urinary retention, central antihypertensives.
- Side effects: Sedation, anticholinergic effects, orthostatic hypotension, cardiac conduction disorders.
- Other antidepressants: Duloxetine.
- Gabapentin (100-300 mg/day at night, up to 3600 mg/day) or pregabalin (150-600 mg/day in 2-3 doses).
- Reimbursed if tricyclics are ineffective or contraindicated.
Second-line:
- Tramadol (50-400 mg/day) and opioids.
- To be avoided with SSRIs (increased risk of serotonin syndrome).
- Valproate, carbamazepine, etc.
Third-line (at this stage, refer to pain management specialists):
- Combination of drugs.
- Clonazepam.
- Tizanidine, baclofen.
- Psychotherapies.
Fourth-line:
- Botulinum toxin injections.
- Physical medicine: External neuromodulation, subcutaneous or intrathecal injections of anesthetics or corticosteroids.
- Intrathecal opioid pumps.
- Surgery: Internal neurostimulation, neurosurgical ablation only for incurable conditions.
Bibliography
Bradley WG et al., Neurology in clinical practice, 5th ed., Butterworth-Heinemann, e-dition, 2007
Bouhassira D et al.,Development and validation of the Neuropathic Pain Symptom Inventory, Pain, 2004 Apr
EMC, Traité de neurologie, Elsevier, 2018