Raynaud syndrome
Last edited on : 22/09/2024
Raynaud syndrome or Raynaud phenomenon is a paroxysmal vascular acrosyndrome characterized by brief episodes of digital ischemia, indicative of functional vasoconstriction or, more rarely, organic vasoconstriction.
It is very common, with a prevalence ranging from 3 to 20% in women and 3 to 14% in men, depending on the series. The vast majority of cases are idiopathic and benign. It rarely requires symptomatic treatment, with the main focus being on identifying the rare secondary forms that require etiological treatment.
Etiologies
- Primary Raynaud = idiopathic = "Raynaud disease" ≈ 90% of cases
- Secondary Raynaud ≈ 10% of cases:
- Iatrogenic and toxic causes: beta-blockers, ergot derivatives, bleomycin, bromocriptine, cyclosporine, interferon alpha, arsenic, cocaine, nicotine, cannabis, LSD, estrogen-progestin, etc.
- Connective tissue diseases, vasculitis and hematological disorders: scleroderma, systemic lupus erythematosus, antiphospholipid syndrome, Sharp syndrome, polymyositis, dermatomyositis, rheumatoid arthritis, Sjögren's syndrome, cryoglobulinemia, cryofibrinogenemia, cold agglutinin disease, HBV-associated vasculitis, Buerger's disease, Takayasu's arteritis, Horton's arteritis, POEMS syndrome, etc.
- Endocrine causes: hypothyroidism, Hashimoto's thyroiditis, acromegaly.
- Non-inflammatory arteriopathies: atherosclerosis, distal embolisms, thoracic outlet syndrome, fibrodysplasia, spastic angina.
- Traumatic causes: working with vibrating tools, ulnar aneurysm, localized repetitive microtrauma (angiography will show aneurysms, stenoses, etc.).
- Miscellaneous: neoplasms, paraneoplastic syndromes, myelodysplasias, glomus tumor, carpal tunnel syndrome, cardiac emboli, arteriovenous fistulas or malformations, pulmonary hypertension, etc.
Diagnosis and Clinical Presentation
Typically, episodes are triggered by cold and/or stress and are divided into three successive phases:
- Syncopal "white" phase (arteriolar spasm): Fingers become white or discolored and numb, lasting from a few minutes to an hour (++ ≈ 15 minutes).
- Asphyxial "blue" phase (venular spasm): Fingers become cyanotic with dysesthesias.
- Hyperemic "red" phase (resolution): Fingers turn red to vermilion, with tingling and significant pain.
However, atypical presentations are common and can complicate the diagnosis:
- Other possible locations: toes, nose, ears, chin, nipples.
- Sometimes only the white phase (up to 30% of cases) and/or blue phase occurs.
- Possible association with acrocyanosis or erythromelalgia.
The progression is always benign in primary Raynaud. In secondary Raynaud, the prognosis depends on the underlying etiology.
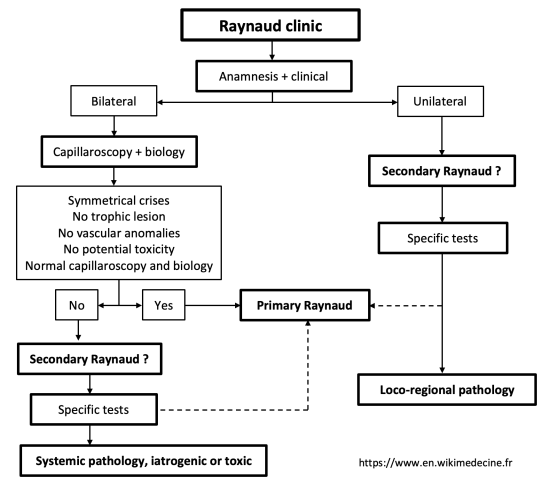
The etiological diagnosis is based on clinical findings and complementary examinations. Features suggesting secondary Raynaud include:
- Absence of a family history.
- Age of onset > 40 years or < 10 years.
- Potential identified iatrogenic/toxic cause.
- Signs of vasculitis or connective tissue diseases (particularly consider scleroderma: periungual or facial telangiectasias, crackles at lung bases, skin sclerosis, trophic disorders, dysphagia, etc.).
- Abnormal capillaroscopy, presence of significant ANA, elevated ESR.
- Abnormal vascular examination or Allen test.
- Unexplained weight loss.
- Trophic lesions → almost always secondary.
- Strictly unilateral (rare) → almost always secondary → consider local-regional pathology (trauma? arteriopathies? atherosclerotic stenosis downstream?).
In scleroderma, Raynaud’s is often the initial manifestation → always consider in the case of atypical features.
Workup
- Systematic examinations:
- Capillaroscopy:
- Normal in primary Raynaud’s.
- Variable abnormalities possible depending on the etiology in secondary Raynaud’s.
- Laboratory tests (ANA, ESR, complete blood count, renal and liver function tests, TSH, RF, C3, C4).
- Urine collection (looking for proteinuria).
- Capillaroscopy:
- Conditional Examinations Based on Clinical Orientation:
- Hand X-rays (subcutaneous calcinosis? Osteolysis?)
- Angiographic studies, Doppler ultrasound, chest X-ray (thoracic outlet syndrome? Signs of pulmonary fibrosis?), nerve conduction velocities (evidence for carpal tunnel syndrome?), etc.
Therapeutic Management - Treatments
- Systematic Measures:
- Control of cardiovascular risk factors (exacerbating factors).
- Smoking cessation.
- Avoidance and protection against cold.
- Avoidance of aggravating toxins and medications.
- Symptomatic Treatment - Limited Evidence-Based Medicine (EBM) → To be considered only in cases of disabling Raynaud and with absolute adherence to contraindications:
- First-line treatment: Calcium channel blockers (e.g., nifedipine 30 mg/day, amlodipine 5 to 10 mg/day, diltiazem, nicardipine, etc.).
- Second-line treatment: Angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor antagonists.
- Third-line treatment: Local nitroglycerin (ointments, gels), iloprost, etc.
- Etiological Treatment in Cases of Secondary Raynaud
Bibliography
EMC, Traité d'Angéiologie, Elsevier, 2014
Creager M et al., Vascular Medicine: A Companion to Braunwald’s Heart Disease, Saunders, 2013