Superficial siderosis
Last edited on : 23/09/2024
Superficial siderosis of the central nervous system (or marginal hemosiderosis) is a chronic clinico-radiological syndrome that combines relatively stereotyped neurological symptoms with the presence of hemosiderin deposits within the leptomeninges and subpial regions.
Although many authors (mostly radiologists...) also use this designation to describe isolated radiological abnormalities, it seems preferable in this case to use the term "radiological siderosis".
Epidemiological elements
The disease is considered rare, if not exceptional, although its prevalence is not determined. However, several elements suggest that it may be underdiagnosed:
- With the progress of MRI, an increasing number of case reports and small series are reported.
- In particular, outside the characteristic clinical triad, many atypical cases (isolated cognitive deterioration, "stroke-like" episodes, isolated progressive deafness, etc.) are reported.
- A large recent series found 0.7% of subjects whose MRI met the radiological criteria (no long-term clinical follow-up) for siderosis in a representative sample of the general population.
- A recent series found radiological siderosis (no long-term clinical follow-up) in over 60% of patients who presented with intraparenchymal hemorrhage in the context of histologically proven cerebral amyloid angiopathy.
- A series found the appearance of radiological siderosis (no long-term clinical follow-up) in the months following, and remaining stable thereafter, a single aneurysmal subarachnoid hemorrhage in over 50% of patients.
It can occur at any age but is more frequently diagnosed between 40 and 70 years old. There is a male predominance (role of more frequent head traumas in men?) in the series.
Pathophysiological elements
The pathophysiology remains uncertain. The currently considered hypothesis is that of subarachnoid hemorrhages, usually occult and repeated, leading to the accumulation of hemosiderin directly and irreversibly neurotoxic under the pial surface (the accumulation of iron favoring the formation of free radicals).
Etiologies
The causes found are those of subarachnoid hemorrhages. Their proportions vary widely depending on the series.
- Idiopathic sideroses (35 to 50% of cases): no source of bleeding found despite adequate assessment
- Secondary sideroses:
- Brain and spinal tumors
- Vascular malformations (aneurysms, arteriovenous malformations, dural fistulas)
- Cerebral amyloid angiopathies, associated or not with Alzheimer's disease
- Head, spinal cord, or brachial plexus traumas, chronic subdural hematomas, and neurosurgical interventions
- ...
Clinical and Prognosis
The characteristic triad consists of the insidious onset of:
- Cerebellar ataxia
- Bilateral sensory deafness
- Myelopathy with pyramidal syndrome. Frequently limited to bilateral hyperreflexia
Also encountered may be: cognitive deterioration, sphincter disorders, para- or tetraparesis, anosmia, headaches, transient "stroke-like" deficits (discussed), sensory disorders, epileptic seizures, optic neuropathies,...
For the least specific symptoms (cognitive deterioration, stroke-like episodes,...), it is not always clear whether the reported clinical manifestations result from siderosis or from other repercussions of the underlying etiology.
→ Typically, the evolution leads to a slow clinical deterioration, frequently towards a bedridden state and death after about ten years, in the absence of etiological treatment. When etiological treatment is possible and performed, the clinical evolution varies (improvement, stabilization, progression).
The risk of occurrence of a hemorrhagic stroke is increased compared to the general population.
Additional examinations
- MRI (entire neuraxis!):
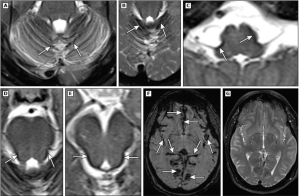
- For positive diagnosis: pathognomonic and highly sensitive T2* sequences → hemosiderin appears as a hypodense rim on the surface of the brainstem, cerebellum, spinal cord, and cerebral cortex. Lower sensitivity of FLAIR and T2 sequences (hypodensities) and T1 (frequently normal or rarely showing hyperintensities). No contrast enhancement.
- Main differential diagnoses: magnetic artifacts, melanosis, meningoangiomatosis
- For etiological research: vascular malformation? fluid collection suggestive of dural breach? amyloid angiopathy? tumor? ...
- For positive diagnosis: pathognomonic and highly sensitive T2* sequences → hemosiderin appears as a hypodense rim on the surface of the brainstem, cerebellum, spinal cord, and cerebral cortex. Lower sensitivity of FLAIR and T2 sequences (hypodensities) and T1 (frequently normal or rarely showing hyperintensities). No contrast enhancement.
- Search for cardiovascular risk factors: echocardiography, ambulatory blood pressure monitoring, laboratory tests including serum lipid levels
- ENT examination with audiometry
- On a case-by-case basis:
- Conventional angiography: for the search of vascular etiologies. Low yield.
- Lumbar puncture:
- Not specific. Possible presence of erythrocytes, increased protein levels, xanthochromic appearance, and pigment presence
- Useful for the diagnosis of some rare etiologies (central nervous system vasculitis) or possible demonstration of ongoing bleeding. Marginal yield.
Therapeutic management - Treatments
There is no evidence-based medicine regarding therapeutic management. However, there is a relative consensus for:
- In case of identified etiology: etiological treatment (endovascular, surgical, radiotherapy, etc.) if possible
- In the absence of identified etiology:
- Control of cardiovascular risk factors. Consider systematic antihypertensive treatment (e.g., indapamide)
- Restrict anticoagulant therapy indications to the maximum extent possible. Be more restrictive regarding the prescription of antiplatelet agents.
- ENT consultation regarding the opportunity to place cochlear implants in cases of deafness
- Consider prescribing low-dose iron chelators on a case-by-case compassionate basis. No evidence-based medicine but some articles report improvement. Prefer deferoxamine, as other chelators have serious potential side effects.
The case of isolated radiological sideroses
There is insufficient data regarding the clinical significance of the incidental discovery (unrelated to clinical symptoms) of radiological siderosis. We can only recommend non-invasive assessment (neuraxis MR angiography and search for cardiovascular risk factors), management of any abnormalities found, and clinical follow-up.
Bibliography
Bradley et al., Neurology in clinical practice, 5th ed., Butterworth-Heinemann, e-dition, 2007
Charidimou A et al., Prevalence and mechanisms of cortical superficial siderosis in cerebral amyloid angiopathy, Neurology, 2013, Aug 13, 81(7):626-32
Kondziella D et al., Diagnostic and therapeutic challenges in superficial CNS siderosis, Dan Med J, 2015 May, 62(5)
Kumar N, Superficial siderosis, Uptodate, 2022
Levy M et al., Superficial siderosis: a case report and review of the literature, Nature Clinical Practice Neurology, (2007) 3, 54-58
Linn J et al., Prevalence of superficial siderosis in patients with cerebral amyloid angiopathy, Neurology, 2010, 74 (17): 1346-50
Linn J et al., Superficial siderosis is a warning sign for future intracranial hemorrhage, J Neurol, 2013, Jan, 260(1):176-81
Lummel N et al., Clinical spectrum, underlying etiologies and radiological characteristics of cortical superficial siderosis, J Neurol, 2015, Jun, 262(6):1455-62
Lummel N et al., Prevalence of superficial siderosis following singular, acute aneurysmal subarachnoid hemorrhage, Neuroradiology, 2015, Apr, 57(4):349-56
Modest MC et al., Cochlear Implantation in Patients With Superficial Siderosis: Seven Cases and Systematic Review of the Literature, Otol Neurotol, 2015, Jun 11
Na HK et al., Cortical superficial siderosis: a marker of vascular amyloid in patients with cognitive impairment, Neurology, 2015, Feb 24, 84(8):849-55
Osborn et al., Diagnostic imaging : brain, Amirsys, USA, 2d ed., 2009
Vernooij MW et al., Superficial siderosis in the general population, Neurology, 2009, Jul 21, 73(3):202-5
Zonneveld HI et al., Prevalence of cortical superficial siderosis in a memory clinic population, Neurology, 2014, Feb 25, 82(8):698-704