Waldenstrom macroglobulinemia
Last edited on : 26/09/2024
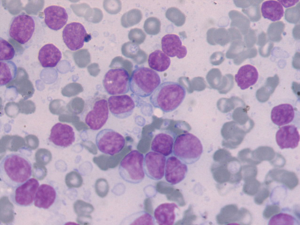
Waldenström disease, or Waldenström macroglobulinemia, is a chronic B-cell lymphoproliferative syndrome characterized by lymphoplasmacytic infiltration of the bone marrow and the presence of a monoclonal IgM-type serum immunoglobulin.
Some consider it to be an evolving form of low-grade non-Hodgkin lymphoma (NHL). It is the first diagnosis to consider in the case of an IgM spike in electrophoresis.
It is a rare disease with an incidence of 0.5 cases per 100,000 inhabitants per year. It accounts for about 2% of malignant hematological diseases. The median age at diagnosis is 63 years, and the sex ratio is 2 females to 1 male.
There are exceptional familial forms, to be investigated in patients under 50 years of age.
Clinical Presentation
In 40 to 50% of cases, the diagnosis is made following the incidental discovery of biological abnormalities (elevated sedimentation rate, abnormal blood count, disturbed electrophoresis). In other cases, and during disease progression, various clinical abnormalities may occur:
- Tumor infiltration signs (30-50%)
- Lymphadenopathy (more frequently cervical-axillary than inguino-crural), typically bilateral, symmetrical, firm, painless
- Hepatosplenomegaly, generally mild (20-30%)
- In 10%: signs of organ infiltration (digestive, bone, pulmonary, renal, neurological, etc.)
- Plasma hyperviscosity signs (~ 15% of cases, due to water molecule binding on carbohydrate residues of IgM and altered red blood cell deformability caused by IgM)
- Hemorrhagic syndrome: epistaxis, gingival bleeding, hematemesis, etc.
- Also due to interaction with coagulation factors, phospholipids, or platelets
- Neurological distress syndrome: headaches, alertness disturbances, neuropathies, etc.
- Hemorrhagic syndrome: epistaxis, gingival bleeding, hematemesis, etc.
- Cryoglobulinemia activity signs (type I or II cryoglobulins present in 10-15% of cases, symptomatic in 5%)
- Raynaud's phenomenon, peripheral vascular occlusions, vascular purpura, arthralgia, recurrent skin ulcers, vascular acrosyndrome, neuropathies, nephropathies, etc.
- Bone marrow failure signs: pallor, weakness, dyspnea
- General signs: weight loss, fatigue
- AL amyloidosis signs (2% of cases) with frequent cardiac and pleuro-pulmonary involvement
- Autoimmune polyneuropathies (anti-MA, anti-GM1, anti-disialosyl, anti-heparin disaccharide activity)
Disease Evolution and Prognosis
The usual course is that of a chronic lymphoid hematologic disorder with successive relapses: elevation of [IgM], progressive development of pancytopenia, infectious complications. ~15% of associated cancers occur. Possible transformation (~5-10%) into aggressive lymphoma.
Median survival is 5 to 10 years with treatment. Complete remission is rare. Main unfavorable factors: age > 60-70 years, anemia, β2-microglobulin > 3 mg/l, albumin < 40 g/l, weight loss, bi- or pancytopenia.
Additional Examinations
- Biology:
- Elevated sedimentation rate (ESR) (cryoglobulinemia can normalize ESR), often normochromic normocytic anemia, rarely lymphocytosis and/or neutropenia, thrombocytopenia (40%)
- Protein levels often 80-120 g/l, cryoglobulinemic activity (15%, mainly type I)
- Β2-microglobulin > 3 mg/l in 50%, cold agglutinin activity in 10%, elevated LDH in aggressive forms, renal/liver function disturbances, frequent coagulation anomalies
- Electrophoresis: IgM spike
- Immunoelectrophoresis/fixation: IgM spike (with κ light chain in 75%)
- Urinalysis: low-level Bence-Jones proteinuria in 50-60% of cases
- Bone marrow aspiration and biopsy:
- Hypercellular marrow with lymphoid, lymphoplasmacytic, or polymorphic plasma cell infiltration (20-100% of cells) and frequent mast cell presence (26% of patients), mild myelofibrosis (50%)
- Lymph node biopsy:
- Diffuse infiltration of lymphoid cells with mast cells, loss of normal architecture
- Lymphoid cell immunophenotyping
- Fundus examination if (suspected) hyperviscosity syndrome
Diagnostic Criteria
Still under debate. Currently, it is considered that the following combination defines the disease:
- IgM monoclonal spike, regardless of its magnitude (however, the higher the level, the more likely the diagnosis)
- Generally diffuse bone marrow infiltration by small lymphocytes with plasma cell differentiation
- Tumor phenotype: IgM+, CD5-/+, C10-, CD19+, CD20+, CD22+, CD23-, CD25+, CD27+, FMC7+, CD103-
Differential Diagnosis
The differential diagnosis of Waldenström's disease includes IgM monoclonal gammopathy:
- Asymptomatic Waldenström's disease
- No treatment required, median progression to symptomatic disease is 7 years
- MGUS with IgM
- Marginal zone lymphomas with monoclonal IgM component
- Difficult differential diagnosis (histological arguments, low IgM spike with other spikes, etc.)
- Chronic Lymphocytic Leukemia
- Generally characterized by hypogammaglobulinemia, but a small IgM spike is observed in 10-15% of cases
- IgM Cryoglobulinemia
- Primary idiopathic cold agglutinin disease
- IgM multiple myeloma: rare
- Secondary IgM monoclonal gammopathies: infections (EBV, CMV, HIV, hepatitis, etc.), autoimmune diseases (SLE, RA, Sjögren's, thyroiditis, PAN), cirrhotic liver diseases, glomerulopathies, etc.
- Randall syndrome, chronic urticaria with IgM (Schnitzler), heavy chain disease, etc.
Therapeutic Management - Treatments
Criteria for starting treatment (symptomatic disease):
- General symptoms (sweats, fever, general deterioration) or symptoms related to IgM's harmful activity (see above)
- Hb < 10 g/l or Platelets < 100.10^9/l or significant tumor mass (reflected by β2-microglobulin levels)
A high IgM level is not a therapeutic criterion but requires thorough investigation of clinical manifestations (hyperviscosity syndrome? retinal hemorrhages or exudates in fundus examination?).
Management is based on symptomatic treatment of complications, plasmapheresis (++ as adjunctive treatment in cases of progressive organ involvement), chemotherapy (chlorambucil, fludarabine, 2CDA with or without monoclonal antibodies), and autologous or allogeneic bone marrow transplants. Although there is no evidence of superiority, these molecules can also be used in combination or combined with an immunosuppressant (cyclophosphamide) or corticosteroids.
Bibliography
EMC, traité d'hématologie, Elsevier, 2018
Jameson JL et al., Harrison's Principles of Internal Medicine, 20th edition, McGraw Hill Higher Education, 2018