Wernicke encephalopathy
Last edited on : 22/09/2024
Wernicke Encephalopathy (or Wernicke's Encephalopathy or Wernicke disease) is a relatively common condition (prevalence of 0.1 to 0.6%) that variably combines confusion, oculomotor disturbances, and balance disorders. It is usually caused by a deficiency in thiamine (vitamin B1). It is most often seen in severely malnourished individuals in developing countries and chronic alcoholics in Western countries.
Of (sub)-acute onset and potentially curable in the early stages, but likely to progress to irreversible Korsakoff syndrome if not properly managed, it is unfortunately underdiagnosed in its early stages. It is frequently associated with beriberi, which shares the same etiologies.
Its mortality rate is around 15% (mainly due to septic and respiratory complications during hospitalization and the decompensation of associated conditions), and the cost of social care for survivors makes it a major public health issue, largely ignored by authorities.
While it is still common for Wernicke's syndrome to be considered by physicians as an exclusive complication of chronic alcoholism, it is important to note that even in Western countries, nearly 50% of cases have a non-alcoholic origin. Moreover, although the average age of onset is 50 years, it can occur in both children and adults and can result from causes other than thiamine deficiency.
Wernicke's encephalopathy is a medical emergency.
Pathophysiological Elements

The human body is unable to produce thiamine and depends on dietary intake. It is stored in only very small amounts by the muscles, nervous system, and liver. In the absence of sufficient external intake, these reserves are depleted in 2 to 3 weeks. Thiamine is the precursor of two bioactive forms necessary for the proper functioning of several metabolic pathways:
- Thiamine pyrophosphate (or thiamine diphosphate, TPP), which is involved in:
- Carbohydrate metabolism and energy reserve production:
- Krebs cycle: TPP catalyzes the oxidative decarboxylations of pyruvate, contributing to the production of acetyl-CoA, and alpha-ketoglutarate, contributing to the formation of succinyl-CoA.
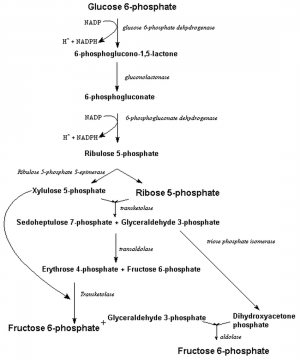
- Pentose phosphate pathway: TPP is also the coenzyme of transketolase, catalyzing the production of fructose-6-phosphate.
- Degradation of pyruvate (see Krebs cycle), whose accumulation leads to the overproduction of lactates (toxic to all cells, but particularly to neurons and glial cells).
- The oxidative decarboxylation of pyruvate (see Krebs cycle) is also a necessary step in the formation of acetylcholine (a neurotransmitter), and that of alpha-ketoglutarate in the formation of gamma-aminobutyric acid (GABA, a neurotransmitter).
- Carbohydrate metabolism and energy reserve production:
- Thiamine triphosphate, whose role is still poorly understood. It is thought to be involved in cell signaling processes and neurotransmission.
Magnesium is an essential cofactor for TPP activity.
A deficiency in TPP or its cofactors therefore leads to cellular distress (energy deficiency), particularly for the nervous system and cardiac muscle (the tissues with the highest energy demand). Some authors suggest a possible individual genetic susceptibility (enzymatic abnormalities in the aforementioned pathways).
Such a deficiency can occur in different situations (isolated or combined):
- Insufficient dietary intake of thiamine
- Impaired intestinal absorption of thiamine
- Impaired phosphorylation of thiamine to TPP
- Physiological or pathological hypermetabolic and hypercatabolic states (overconsumption of TPP)
- Increased urinary excretion of thiamine
- Presence of compounds neutralizing thiamine (thiaminases)
- Severe hypomagnesemia
Anatomopathological Elements
Histologically, Wernicke's syndrome is characterized by a variable combination of gliosis, neuronal loss, hemorrhagic petechiae, and necrotic areas within the mammillary bodies, the periventricular regions of the midbrain and brainstem, the thalamus, and the hypothalamus.
According to the etiology, other lesions may be observed (e.g., for chronic alcoholism: brain and cerebellar atrophy, typical lesions of Marchiafava-Bignami disease, hepatic encephalopathy, etc.).
Epidemiological Elements
The clinical prevalence of Wernicke's syndrome is estimated in developed countries to be between 0.1% and 0.6%.
Autopsy series describe typical Wernicke-Korsakoff lesions in 0.4% to 2.8% of autopsies in the general population, 12.5% of autopsies in chronic alcoholics, and > 50% of patients whose deaths are attributed to alcohol-related complications.
Radiological prevalence (MRI series) is intermediate between clinical and autopsy prevalences.
This disparity between clinical prevalence and radiological or autopsy prevalence suggests that up to 80% of cases may go undiagnosed... although some cases may be asymptomatic or minimally symptomatic.
Epidemiological data in developing countries are unknown. However, the condition is typically considered more common there due to high rates of malnutrition.
Etiologies
- In developing countries: undernutrition and malnutrition are considered nearly exclusive causes. However, epidemiological data are sparse.
- In developed countries:
- Chronic alcoholism is the predominant cause (present in > 50% of cases).
- Possible mechanisms include: frequently inadequate dietary intake in alcoholics, intestinal absorption disorders due to alcohol’s digestive toxicity, increased carbohydrate metabolism (which consumes thiamine) caused by alcohol, thiamine metabolism defects (hepatic cell insufficiency), increased incidence of hypomagnesemia and other predisposing pathologies.
- Various (rare causes considered individually but totaling nearly 50% of cases overall):
- Restrictive or unbalanced diets, anorexia, pregnancy and breastfeeding, parenteral nutrition without supplementation, malnutrition, gastrointestinal surgery, cancers, transplants, dialysis, acquired immune deficiency syndromes, persistent vomiting or diarrhea, hepatic cell insufficiency, prolonged febrile and hypercatabolic or hypermetabolic states (hyperthyroidism, etc.), inappropriate infusions, severe hypomagnesemia, polyuric and diuretic syndromes, etc.
- These etiologies can lead to Wernicke's syndrome alone, in combination, or on a background of chronic alcoholism.
- Chronic alcoholism is the predominant cause (present in > 50% of cases).
Clinical Presentation
Syndromic triad (rarely fully present):
- Confusion, altered consciousness. Deep consciousness disturbances such as coma or progression to death are exceptional.
- ++ Ataxia (balance and gait disorders).
- Oculomotor disturbances (++ gaze nystagmus, third cranial nerve involvement, sixth cranial nerve involvement, etc.).
Other signs and symptoms may include: vestibular disorders, hypothermia, tachycardia, orthostatic hypotension, syncope, etc.
In the majority of cases, beriberi is also associated: signs of acute polyneuropathy (rapidly developing distal paresis and hyporeflexia) and/or (sub)-acute heart failure (effort or resting dyspnea, lower limb edema, etc.).
Finally, one should look for signs of nonspecific complications (++ sepsis, traumatic complications from falls, etc.) and other nutritional deficiencies.
Differential Diagnosis, Associated Pathologies, and Boundaries of the Pathology
When the clinical picture includes at least two syndromic signs in an evocative context (chronic alcoholism, diet, malnutrition, etc.), a positive diagnosis is relatively easy to establish. In other cases, the differential diagnosis is broad, including encephalopathy (with particular attention to deficiency and withdrawal syndromes), oculomotor disorders, or ataxia (see specific chapters).
In addition to general complications and those specific to the etiology, various other deficiency-related pathologies with (sub)-acute onset are frequently associated (and, in some cases, represent a differential diagnosis) with Wernicke's syndrome. Since these pathologies share overlapping semiological features, their identification is often challenging.
Beriberi
See detailed article: Beriberi
Beriberi is a syndrome that variably associates a sensorimotor polyneuropathy and a (sub)-acute dilated cardiomyopathy.
It results from the same etiologies and pathophysiological processes as Wernicke's syndrome and is therefore frequently associated with it.
The syndromic separation between Wernicke's and beriberi is mainly due to historical reasons and can lead to medical errors. Clinicians should consider them as the same pathological entity.
Acute Ethyl-(Deficiency) Polyneuropathies
See detailed article: Ethyl-Deficiency Polyneuropathies
While the existence of acute polyneuropathies (characterized by a variable combination of ataxia, sensory disorders, and distal paresis... which in some cases can result in a flaccid paraplegia mimicking cauda equina or conus medullaris syndrome) in the context of chronic alcoholism is well documented, the pathophysiology is still debated. It is not clear whether these cases should all be classified as forms of beriberi (thiamine deficiency) or if some are due to other vitamin deficiencies or direct neurotoxicity from alcohol... or a combination of these factors. In practice, management involves alcohol withdrawal and multivitamin supplementation.
Pellagra
Pellagra, resulting from a deficiency in nicotinic acid (= niacinamide = vitamin B3 or PP), is characterized by a variable association of gastroenterological manifestations (anorexia, stomatitis, transit disorders, etc.), neurological manifestations (irritability, behavioral disorders, cognitive disorders, confusion, etc.), and cutaneous manifestations (erythematous rash, hyperkeratotic lesions, areas of hyperpigmentation). Early manifestations are often non-specific, limited to neuropsychiatric and/or non-specific gastroenterological symptoms.
It can present alone or in association with Wernicke's syndrome and preferentially occurs in the context of chronic alcoholism and/or malnutrition.
Marchiafava-Bignami Encephalopathy
See detailed article: Marchiafava-Bignami Encephalopathy
Vitamin B12, Folate, Copper Deficiency Syndromes
See detailed article: Acquired Hypocupremia
Alcoholic and/or Deficiency Myopathies
See detailed article: Alcoholic Myopathies
Ethyl-Tobacco and Deficiency Optic Neuropathies
Acute Alcohol Intoxication and Ethyl Withdrawal Syndrome
See detailed article: Acute Alcohol Intoxication
See detailed article: Ethyl Withdrawal Syndrome
See detailed article: Preparing for Ethyl Withdrawal
Protein-Calorie Malnutrition Syndromes
Discovery Circumstances, Iatrogenicity, and Prevention
Unfortunately, it is common for Wernicke's syndrome to be diagnosed only late, during a period of confusion persisting during hospitalization without explanation. The administration of glucose infusions without adequate supplementation is also a frequent cause or contributing factor.
Given that this syndrome is frequent, severe, often irreversible, and easily preventable through vitamin supplementation, the latter should be systematically considered for:
- Oral supplementation (e.g., thiamine 300 mg/day) long-term: all chronic alcoholics and malnourished patients, those with malabsorption, those who have undergone bariatric surgery, etc.
- Intravenous supplementation (see below: treatments) before enteral transition:
- Any chronic alcoholic, malnourished, or malabsorptive patient requiring infusion or re-nutrition. This should also be discussed for some at-risk patients (e.g., cancer patients).
- Any confused patient or those with (sub)-acute onset balance disorders without an obvious explanation.
- Any hospitalized patient in a prolonged hypermetabolic or hypercatabolic state (++ intensive care patients).
Public health policy: combating alcoholism, malnutrition, and inappropriate diets.
Additional Tests
The positive diagnosis of Wernicke's syndrome is exclusively clinical. The reasoned use of additional tests is only justified to exclude potentially treatable differential diagnoses, exclude some non-ethylic etiologies, or assess the impact of comorbidities.
- Blood Biology and Urine Analysis
- The serum concentration of thiamine is generally decreased (variable depending on the etiology). However, this test is not routinely performed (it requires sampling before any vitamin supplementation, very few laboratories conduct this test, thiamine degrades easily requiring strict storage conditions and rapid analysis, treatment should not await results, a positive result does not exclude other clinical causes, and a negative result does not formally exclude Wernicke's syndrome [see pathophysiology elements]).
- It is systematically justified at admission to assist in differential diagnosis (hematology-CRP, electrolyte levels, renal and hepatic functions, vitamin B12 and folates, etc.) and to search for etiologies or aggravating factors (electrolytes, TSH, etc.).
- Electroencephalogram (EEG)
- It is systematically justified to exclude a non-convulsive status epilepticus as a differential diagnosis.
- Lumbar Puncture (LP)
- No interest for positive diagnosis: may show moderate (non-specific) hyperproteinorachia (<100 mg/dl).
- Given its semi-invasive nature, it should only be performed in the presence of fever, meningeal signs, or atypical clinical presentation for differential diagnosis.
- Brain Imaging
- MRI can aid in positive diagnosis: bilateral lesions (hemorrhages, necroses, edema) visible (sensitivity ≈ 50%, specificity ≈ 90%) in T1, T2, T2*, FLAIR, and DWI sequences (++ T2/FLAIR hypersignals regressing with therapeutic response). ++ Mammillary bodies, periphery of the third ventricle, thalamus, and hypothalamus.
- Depending on the clinical presentation, CT or MRI can exclude differential diagnoses (e.g., subdural hematomas, strokes, patterns of various metabolic encephalopathies, etc.) or reveal characteristic lesions of associated pathologies (e.g., hepatic encephalopathy, Marchiafava-Bignami, etc.).
- Electrocardiogram (ECG) and Cardiac Echography
- Should be performed systematically to exclude an associated deficiency-related dilated cardiomyopathy (beriberi) requiring cardiological assessment.
- Others
- Depending on clinical presentation or results from previous tests.
Therapeutic Management - Treatments
Given its relative safety, this treatment should be initiated at the slightest suspicion of diagnosis (particularly in any confused or unexplained gait disorder in an alcoholic or malnourished patient):
- Vitamin Supplementation. Example Scheme:
- Thiamine (B1): 500 to 1500 mg/day IV for 5 days, then switch to PO for a minimum of 3 months
- Other B Vitamins (for associated deficiencies and differential diagnoses):
- Pyridoxine (B6): 500 mg/day IV for 5 days. Maintenance dose < 100 mg/day PO (or high-dose courses at non-specified intervals).
- Nicotinamide (B3, PP): 3 x 100 to 200 mg/day PO or 3 x 25 mg/day IV. Duration not specified before dose reduction.
- Cobalamin (B12): 1 mg/day IM for 7 days (then 1 x/week for 1 month, then 1 x/month)
- Folic Acid (B9): 5 mg/day PO until normalization of serum levels, then 1 mg/day
- Rehydration
- Correction of Etiological/Aggravating Factors: Addressing ionic (particularly correcting any hypomagnesemia) and metabolic disorders
- Management of Associated Manifestations and Complications as needed
- In Case of Chronic Alcoholism: Prevention of alcohol withdrawal syndrome
If Sequelae Persist After Appropriate Medical Management: Only paramedical measures can be proposed according to their severity (gait maintenance physiotherapy, prismatic glasses, social support, placement, symptomatic psychiatric care, etc.).
Note:
- There is little evidence regarding the doses and duration of supplementation. Only the benefit of doses greater than 100 mg/day IV for 3 days of thiamine has been demonstrated, with 500 mg being the consensus minimum in official American recommendations.
- There are no known complications from the usual oral administration of thiamine. High-dose IV thiamine administration complications are rare (e.g., anaphylactic reactions, hemodynamic disturbances, glycemic imbalances).
- Long-term oral administration of pyridoxine at doses > 200 mg/day may lead to irreversible sensory-motor polyneuropathies. It is recommended not to exceed 100 mg/day for long-term use, with preparations like Befact only for short-term courses (e.g., 3 months).
- Cobalamin administration is also possible IV slowly or PO, and folic acid IV at the same doses, though less well-studied.
- Nationally available products may not always allow for adequate supplementation in all situations. In such cases, request the hospital pharmacy to prepare the necessary magistral preparations IV, IM, or PO.
Prognosis
Vitamin supplementation should be started as early as possible to hope for reversibility.
The mortality rate is approximately 15% (due to septic complications, respiratory issues, or associated beriberi cardiac conditions). Persistence of sequelae is the rule even with adequate management: in cases of encephalopathy → only 20% have significant recovery. In cases of recovery, ocular signs regress within hours to days, encephalopathy and ataxia within days to weeks. Symptoms persisting beyond 4 months (the latest documented recovery) are generally considered permanent and usually result in a Korsakoff syndrome.
Bibliography
Bradley WG et al., Neurology in clinical practice, 5th ed., Butterworth-Heinemann, e-dition, 2007
EMC, Traité de neurologie, Elsevier, 2018
Guilland JC, Vitamines hydrosolubles (I). Thiamine, riboflavine, niacine, acide pantothénique, vitamine B6 et biotine, Encyclopédie Médico-chirurgicale, Endocrinologie-Nutrition[10-546-A-10], Elsevier, Paris, 2012
Pazirandeh S et al., Overview of water-soluble vitamins, UpTodate, 2018
Yuen T So, Wernicke encephalopathy, UpToDate, 2022
World Health Organization (WHO) and United Nations High Commissioner for Refugees (UNHCR), Thiamine deficiency and its prevention and control in major emergencies, WHO, 1999




